PARTIAL KNEE REPLACEMENT
POSTERIOR CRUTIC LIGAMENT LIGAMENTOPLASTY (PCL)
Unicompartmental knee replacement is a treatment option for patients with severe osteoarthritis localized to only one part of the knee, usually the medial (inner) compartment or lateral (outer) compartment of the joint. Unlike total knee replacement, which replaces the entire knee joint, unicompartmental replacement involves replacing only the damaged part of the knee.
Here are some key points regarding unicompartmental knee prosthesis:
- Indications : It is generally recommended for patients with severe isolated osteoarthritis in a single compartment of the knee, who have good ligamentous stability and a satisfactory range of motion. Selected patients must also have a moderate body weight and good general health.
- Surgical procedure : Implantation of a unicompartmental knee prosthesis is a less invasive surgical procedure compared to a total knee prosthesis. It requires a smaller incision and less extensive resection of bone and soft tissue.
- Advantages : Potential advantages of the unicompartmental prosthesis include faster recovery, more natural range of motion, feeling closer to the non-operated knee, less blood loss during surgery, and reduced risk of complications such as infection and joint stiffness.
- Limitations : This procedure may not be suitable for all patients, particularly those with evidence of osteoarthritis in multiple compartments of the knee or significant ligamentous instability. Additionally, there is a risk of long-term revision, as a unicompartmental prosthesis may wear out more quickly than a total knee prosthesis.
- Recovery : Recovery after unicompartmental knee replacement surgery varies from patient to patient, but is generally faster than that of a total knee replacement. Rehabilitation exercises are often recommended to strengthen surrounding muscles and improve joint stability.
Unicompartmental knee replacement is an effective treatment option for patients with severe osteoarthritis localized to a single compartment of the knee, providing benefits such as faster recovery and more natural range of motion compared to a total knee replacement. of the knee. However, it is not suitable for all patients and has limitations specific to each case.
WHAT IS THE PROBLEM ?
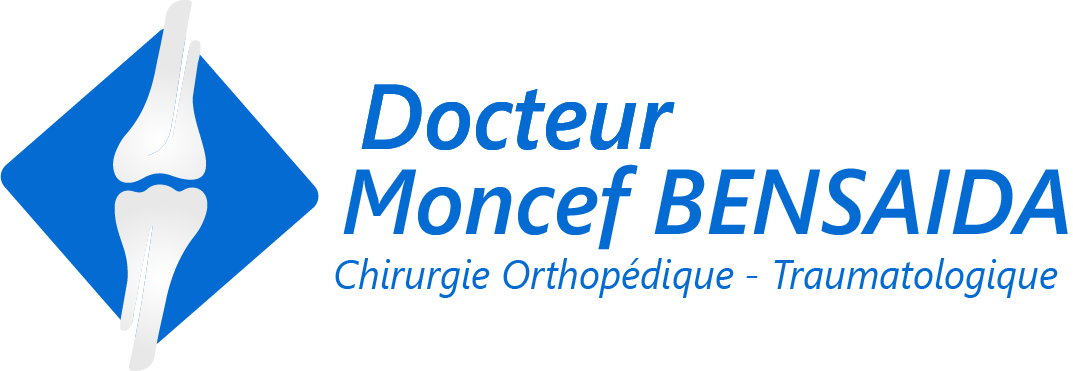
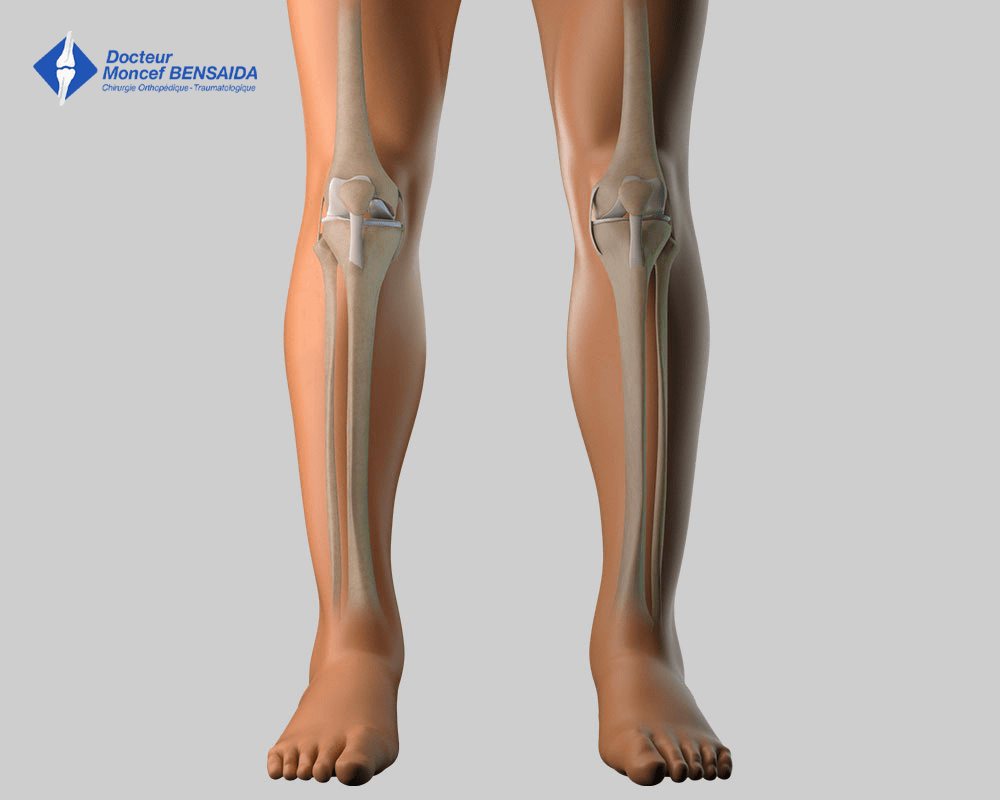
The knee is a complex joint comprising three bones: the femur, the tibia and the patella and not one but three joints:
- the patellofemoral joint between the distal end of the femur and the patella
- the medial femorotibial joint between the medial femoral condyle and the medial tibial plateau
- the lateral femorotibial joint between the lateral femoral condyle and the lateral tibial plateau
Like all joints, the knee is covered with cartilage, a slippery substance with no nerve endings that allows the joint to move freely and painlessly. This cartilage can wear for different reasons (osteoarthritis, bone necrosis, sequellae of a fracture or an infection…) exposing the underlying bone, which is rough and innervated; the joint gradually becomes stiff and painful.
WHEN SHOULD A PARTIAL KNEE REPLACEMENT (PKR) BE CONSIDERED?
When medical treatments (analgesics or injections) no longer relieve the pain, a partial knee replacement is necessary to replace the worn cartilage. When the cartilage wear is restricted to one of the femorotibial compartments and the cartilage is healthy in the rest of the knee, a partial knee replacement (PKR) is possible.
Osteoarthritis of the medial femorotibial compartment
With a partial knee replacement or partial knee resurfacing, postoperative recovery of knee mobility is faster and bone resection is minimal compared to a total knee replacement (TKR). However, there are some contra-indications (obesity, ligament problems, impossibility of totally straightening the knee…) and a total knee replacement (TKR) is thus preferred.
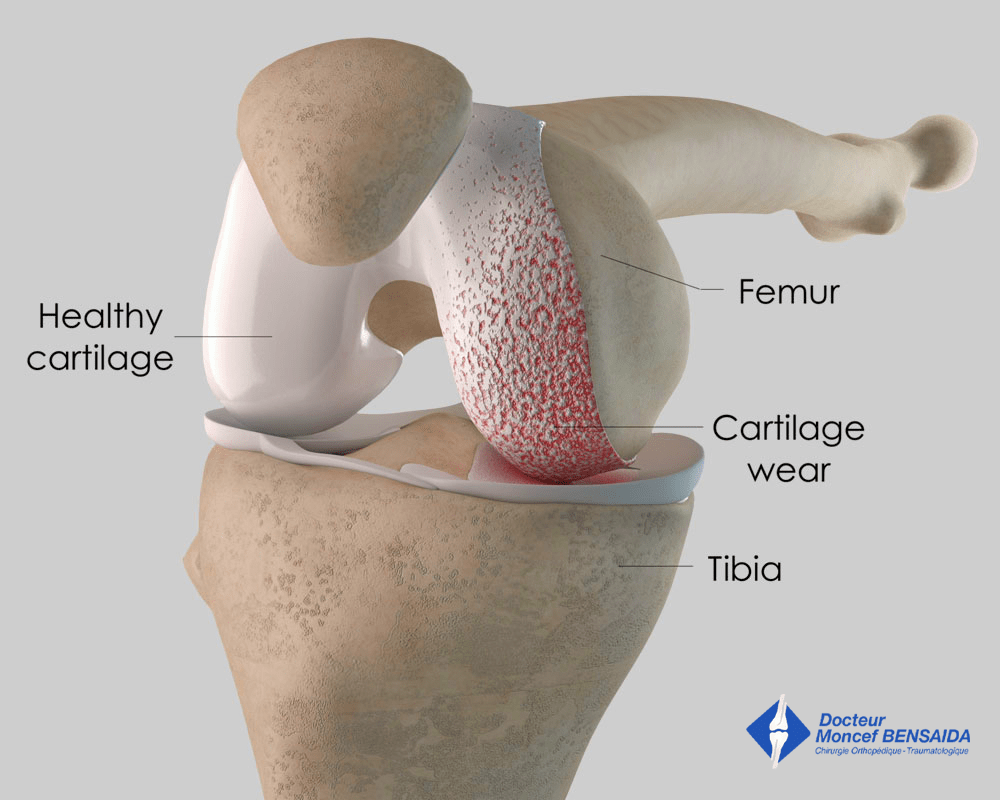
A partial knee prosthesis comprises :
- a femoral implant
- a tibial implant
- a polyethene (plastic) insert placed between the femoral and tibial implants
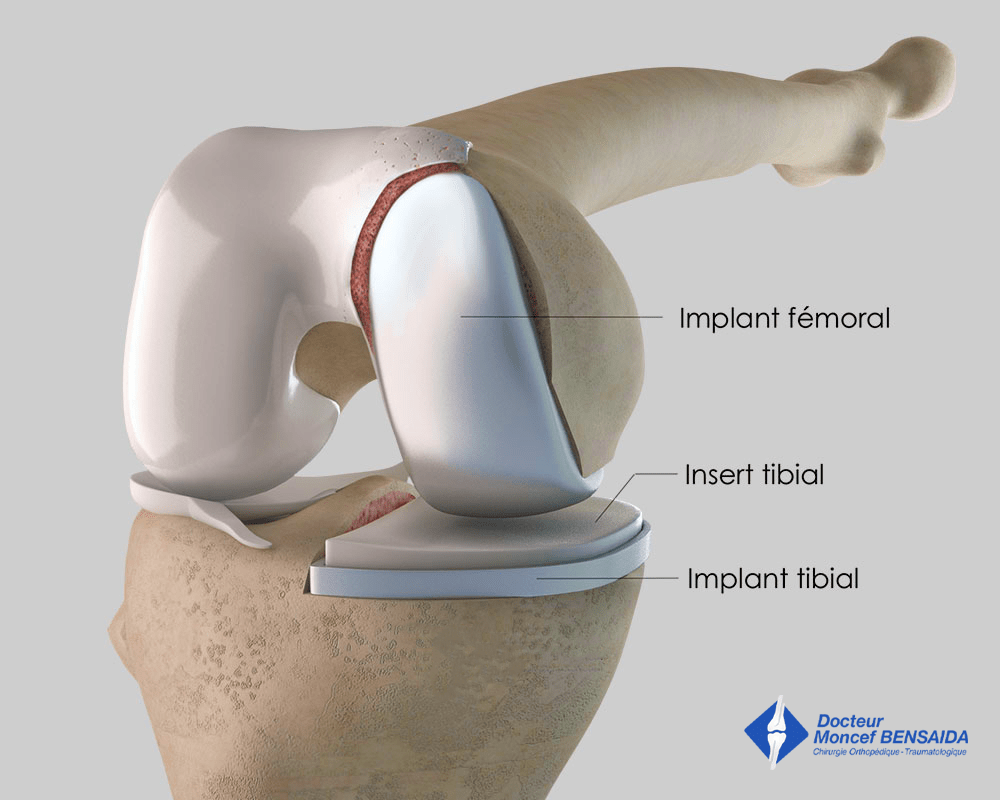
Partial medial replacement
Total knee replacement
BEFORE THE OPERATION
A total knee replacement requires an operation. The implant best suited to the patient is chosen during the pre-surgical consultations. Before the operation, a pre-anaesthesia consultation and a preoperative assessment are conducted to check the patient is physically apt to undergo the operation and minimise the risk of postoperative complications, especially infections. This assessment generally includes a blood test, a cardiovascular check-up, as well as a dental check-up and a urine test to ensure there are no infections and thus avoid any microbial contamination of the implants.
THE OPERATION
The operation takes place in an operating theatre in compliance with strict standards of cleanliness and safety. The patient is placed supine on an operating table and a tourniquet is sometimes placed around the thigh. The operation lasts about 1 hour, sometimes longer in more complex cases.
This operation can be carried out under general or spinal anaesthesia. The latter is a regional anaesthetic anaesthetising the lower part of the body (as with an epidural). The anaesthetist will decide on the most suitable anaesthetic together with the patient.
A partial knee replacement requires an incision on the anterior side of the knee that is generally between 8 and 10 centimetres.
AFTER THE PROCEDURE
After the operation, the knee is partially numbed with a nerve block to help improve postoperative pain management.
The effect lasts approximately 18 hours after the operation but can be extended with the insertion of a catheter in the thigh if the anaesthetist considers it necessary. Medication and ice on the knee also provide effective postoperative pain management.
Partial medial knee replacement
Rehabilitation begins the day after the operation with the help of physiotherapists. Weight-bearing on the limb operated on is allowed from the outset. Crutches are used to start with but are gradually abandoned.
The stay in hospital varies between 1 and 4 days. In some cases, the operation can be carried out as an outpatient procedure. When leaving the clinic, the patient can return home and rehabilitation will continue with a local physiotherapist with 2 to 3 sessions a week for about 1 month. If the patient’s home is too difficult to access or if the patient has no help with daily activities (shopping, meals…) a stay of generally 1 month at a rehabilitation centre can be considered.
When the patient is discharged from the clinic, a consultation with follow-up x-rays of the implant is scheduled with the surgeon 4 to 6 weeks after the operation to check the patient has recovered good gait and good knee mobility. A second check-up is generally recommended approximately 3 months after the operation. Subsequently, x-rays to monitor the replacement are recommended, generally every 2 years, to check there is no wear of the different components or the surrounding bone.
RISKS LINKED TO THE OPERATION
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics. Some infections may require the implants to be replaced.
Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. However, in the case of severe bleeding during or following the operation, another operation to stop the haemorrhage or a blood transfusion may be required.
Knee surgery also increases the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections or tablets) are prescribed for the entire month following the operation.
In rare cases, the knee remains stiff, hot, and painful for several months after the operation. This complication, known as algodystrophy or Chronic Regional Pain Syndrome (CRPS), is unpredictable and sometimes takes a long time to heal.
Finally, rarer complications can also occur. Blood vessels (arteries, veins) can be accidentally damaged and will require vascular surgery (bybass). Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
A FEW QUESTIONS ABOUT PARTIAL KNEE REPLACEMENTS
What is the desired outcome of a partial knee replacement?
A partial knee replacement aims to restore satisfactory function of the knee joint. The aim is two-fold: eliminate the pain and restore joint mobility. A knee replacement helps recover satisfactory, painless walking. However, the range of motion of an artificial knee is lower than a normal knee and is often between 110° and 130°, which enables normal walking even on stairs. Additionally, it is often uncomfortable to kneel on a hard floor with a knee replacement, which can hinder some activities.
Can we forget that we have a knee prosthesis?
Contrary to a hip replacement, it is rare that patients totally forget they have a knee replacement. Indeed, even if the knee is painless, odd feelings are often experienced especially when the weather changes but no specific treatment is required.
A TKR or a PKR?
You do not have to choose as these two types of replacement have clearly different indications (limited cartilage wear for a PKR and diffuse wear for a TKR) and some contra-indications (obesity or extension deficit of articular origin for PKR). The surgeon will decide on the most suitable implant for the patient.
Can the deterioration of knee osteoarthritis be slowed to delay the need for a total knee replacement?
In some cases, conservative surgery (with no implant), of which the aim is to modify the mechanical load on the knee, can slow the progression of moderate, localised knee cartilage wear. The knee axis is modified slightly by realigning the proximal end of the tibia (high tibial osteotomy) or the distal end of the femur (distal femoral osteotomy). This transfers the load from the worn femorotibial compartment to the healthy femorotibial compartment. This type of operation does not heal the worn cartilage but slows the wear and thus delays the need for a knee replacement, which is why it is sometimes proposed to patients under 60 years.
My knee has been hurting for years. Do I need a knee replacement?
A knee replacement is a functional procedure and therefore not compulsory. Only the patient can say if the discomfort is considerable enough to justify an operation. However, before considering surgery, it is necessary to try relieving the pain with medicinal treatments (analgesics, hyaluronic acid injections). In young patients, conservative surgery is sometimes possible to delay a knee replacement.
What is the lifespan of a partial knee replacement?
Today it is reasonable to say that the lifespan of a partial knee replacement is approximately 15 to 20 years, sometimes longer, sometimes shorter. It depends on the level of activity and the weight of the patient.
Furthermore, a partial knee replacement does not prevent the wear of the remaining cartilage in the other knee compartments. However, if debilitating osteoarthritis develops in the rest of the knee, a total knee replacement is possible in good technical conditions.
Am I too young to have a total knee replacement?
Behind this question lies the issue of the lifespan of the implant and the potential need for a revision knee replacement, as it is more complicated and the functional result is not likely to be as good as the primary replacement. It is, therefore, preferable to carry out knee replacements on patients who are never likely to have it changed, in other words, those over 65 years. Nevertheless, this is not set in stone. It is better to have a knee replacement at an age when you can enjoy it rather than delaying the procedure indefinitely and having to suffer the pain and the frustration of restricted mobility. So, for subjects under 50 years with knee damage (sequelae of trauma, for example), it is better to undergo a knee replacement to recover satisfactory function rather than continuing to suffer from the pain for several years and finally undergoing a knee replacement a few years later.
What is the implant made of?
Knee implants are made from inert biocompatible materials, so the risk of an allergy or rejection is exceptional. The metal parts of the implants are alloys, more often than not cobalt-chromium or titanium. Cementless implants are generally coated in osteoconductive materials to facilitate growth of the bone in contact with the implant. The bearing surfaces of the implants, that is the contact surfaces between the implants, are generally metal on polyethene (plastic).
Do I need to make any changes at home after a knee replacement?
No, it is not necessary. However, ground-floor accommodation would be more comfortable in the first few weeks after the operation.
Where will the scar be?
The scar is on the anterior surface of the knee and is generally 8 to 10 cm.
How long does it take to recover your independence?
Satisfactory independence is often recovered after 3 to 4 weeks.
How long after my operation can I travel again?
You have to wait approximately 2 to 3 months before taking a long journey in good conditions (carrying luggage, shuffling during visits…)
When can I drive after the operation? Can I travel by car?
You will generally have to wait 4 weeks after the operation before driving again. When driving again, you must be able to do an emergency stop. You can travel as a passenger earlier but journeys are often uncomfortable due to the low sitting position and it is better to restrict the frequency and more particularly the duration.
How long will I be off work after the operation?
It depends on your profession and the level of physical activity required. It generally varies between 1 and 3 months.
Can I do any sport with a knee prosthesis?
Yes, but it is better to opt for non-weight-bearing sports rather than high-impact sports. Cycling and swimming are therefore better and running should be avoided. To be on the safe side, sport is generally not resumed before the 3rd month after the operation.
What are the risks linked to a total knee replacement?
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics. Some infections may require the implants to be replaced. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. However, in the case of severe bleeding during or following the operation, another operation to stop the haemorrhage or a blood transfusion may be required.
Knee surgery also increases the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections or tablets) are prescribed for the entire month following the operation.
In rare cases, the knee is stiff, hot, and painful for several months after the operation. This complication, known as algodystrophy or Chronic Regional Pain Syndrome (CRPS), is unpredictable and sometimes takes a long time to heal.
Finally, rarer complications can also occur. Blood vessels (arteries, veins) can be accidentally damaged and will require vascular surgery (bypass). Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.