ARTHROSCOPIC CAPSULOLABRAL REPAIR
(BANKART PROCEDURE)
WHAT IS SHOULDER INSTABILITY?
Shoulder instability is a medical condition characterized by an imbalance or excessive laxity of the stabilizing structures of the shoulder joint. The shoulder joint is a very mobile joint that allows for a wide range of motion, but this increased mobility also makes the shoulder more prone to instability.
There are two main types of shoulder instability: anterior instability and posterior instability.
- Anterior shoulder instability: This is the most common form. It occurs when the head of the humerus (the upper arm bone) moves forward in relation to the glenoid socket of the scapula. This may be the result of an injury, torn ligaments, or loosening of the stabilizer muscles.
- Posterior shoulder instability: Less common, this form occurs when the head of the humerus moves posteriorly relative to the glenoid socket.
Causes of shoulder instability may include traumatic injuries, ligament tears, congenital laxity, muscle weakness, or overuse of the shoulder. Common symptoms may include pain, sensations of dislocation or subluxation, and limitations in shoulder movement.
Treatment for shoulder instability may vary depending on the severity of the condition and symptoms. It may include muscle strengthening exercises, rehabilitation, changes in physical activity, or in more severe cases, surgery to stabilize the joint. It is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan if shoulder instability is suspected.
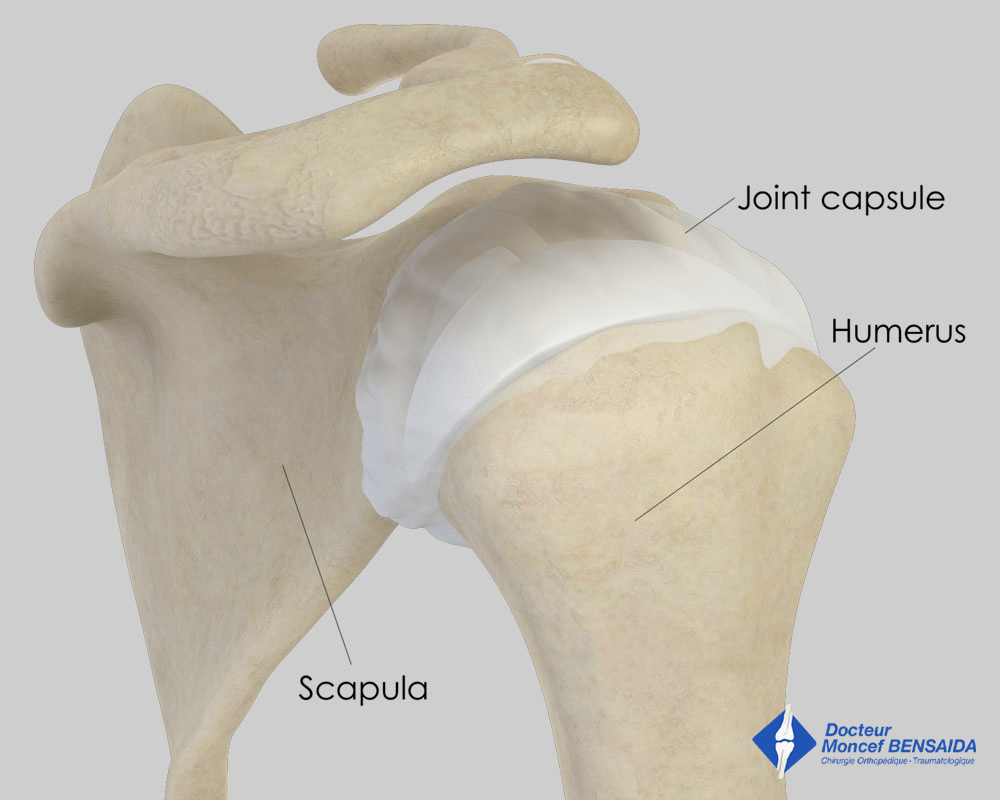
Normal shoulder (posterior view)
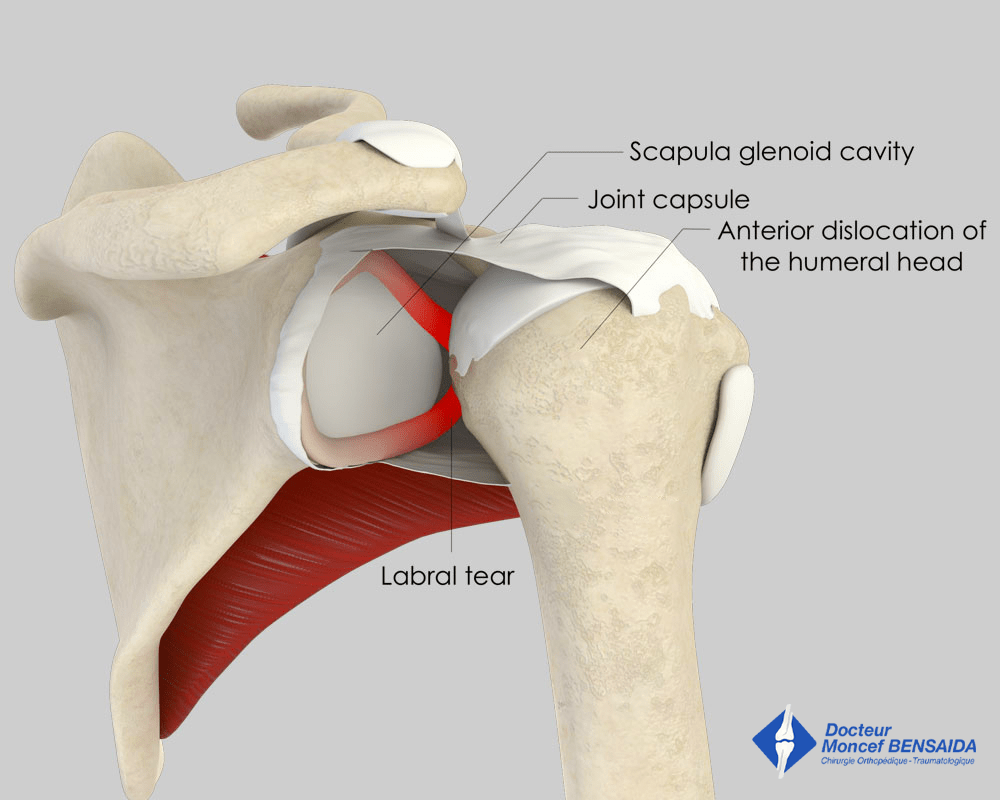
Anterior shoulder dislocation
WHAT ARE THE CONSEQUENCES OF SHOULDER INSTABILITY?
Shoulder dislocations damage the anatomical components ensuring joint stability: ligaments, labrum. Furthermore, fractures of the head of the humerus or the glenoid can occur during dislocations.
These dislocations decrease shoulder stability and increase the risk of relapses. This is known as chronic instability or recurrent dislocation.
WHEN SHOULD YOU CONSULT?
Shoulder instability can be an issue when doing some sports such as swimming, handball or tennis, and dislocations can occur during competitions. Patients who have dislocated their shoulder several times often develop apprehension when cocking their arm; they are very wary of putting their arm up and back in case the shoulder dislocates.
Sometimes, after one or several dislocations, there is no apprehension but the shoulder is painful. This is referred to as a unstable painful shoulder.
When the apprehension or the pain becomes troublesome, it can be useful to consult to assess the damage and look at possible treatments.
WHAT EXAMINATIONS ARE NECESSARY?
The different examinations aim to assess the damage caused by the dislocations and choose the most suitable operation to stabilise the shoulder.
The examinations must include x-rays to see if there are any fractures of the glenoid or the head of the humerus. A CT arthrogram, which is a scan with the injection of an x-ray contrast medium in the shoulder, is often performed as well to visualise any damage to the labrum.
WHAT IS THE BANKART PROCEDURE?
With recurrent dislocations that disrupt work-life or sports activities, a Bankart procedure can be proposed. This operation restores shoulder stability in the case of anterior dislocation.
This operation is carried out arthroscopically, a minimally invasive technique, through 2 to 3 incisions 5 millimetres long around the shoulder and consists in repairing the torn labrum and tightening the joint capsule, which is the envelope surrounding the joint.
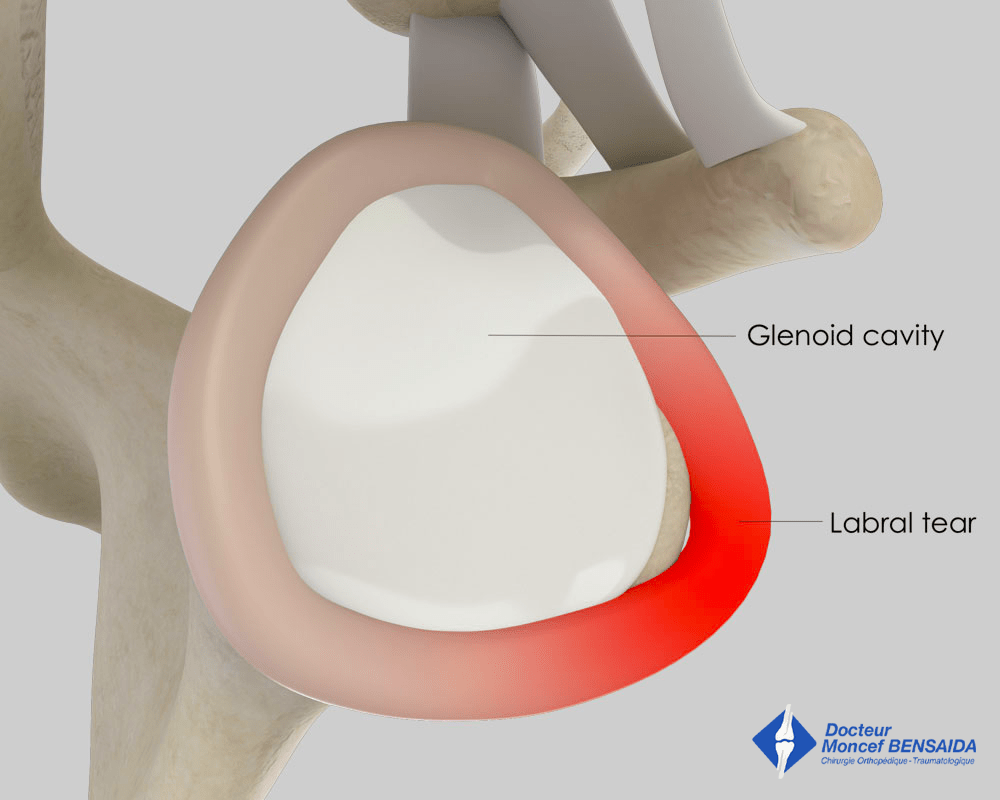
Labrum avulsion (side view)
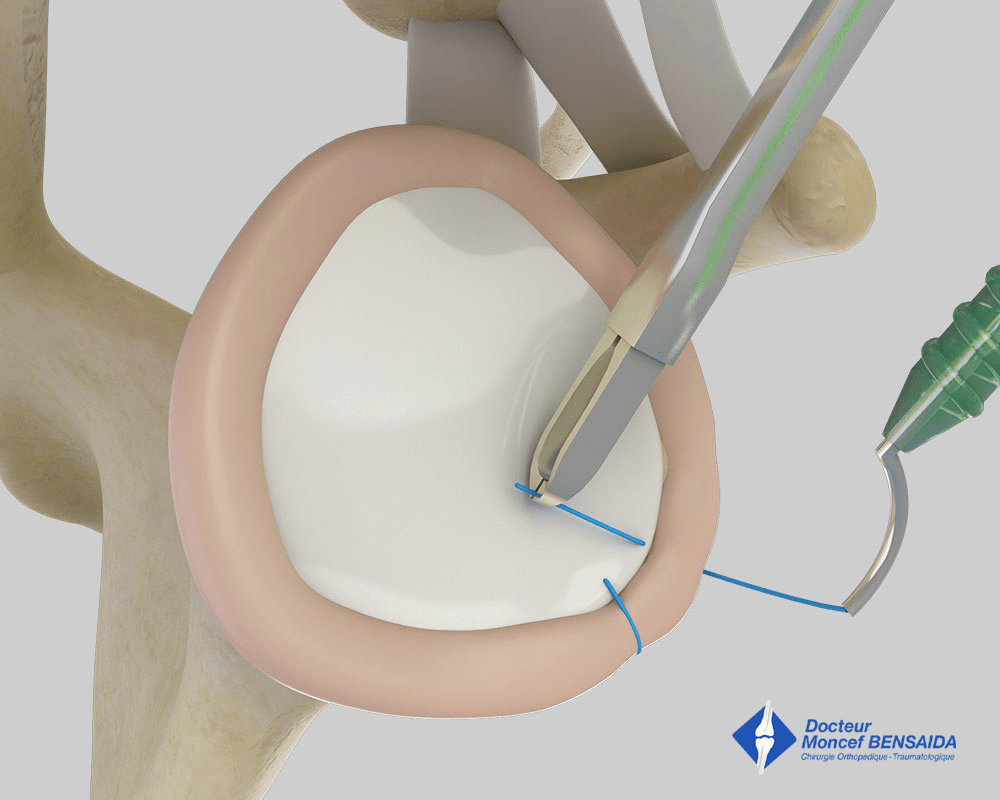
Arthroscopic reinsertion of the labrum (side view)
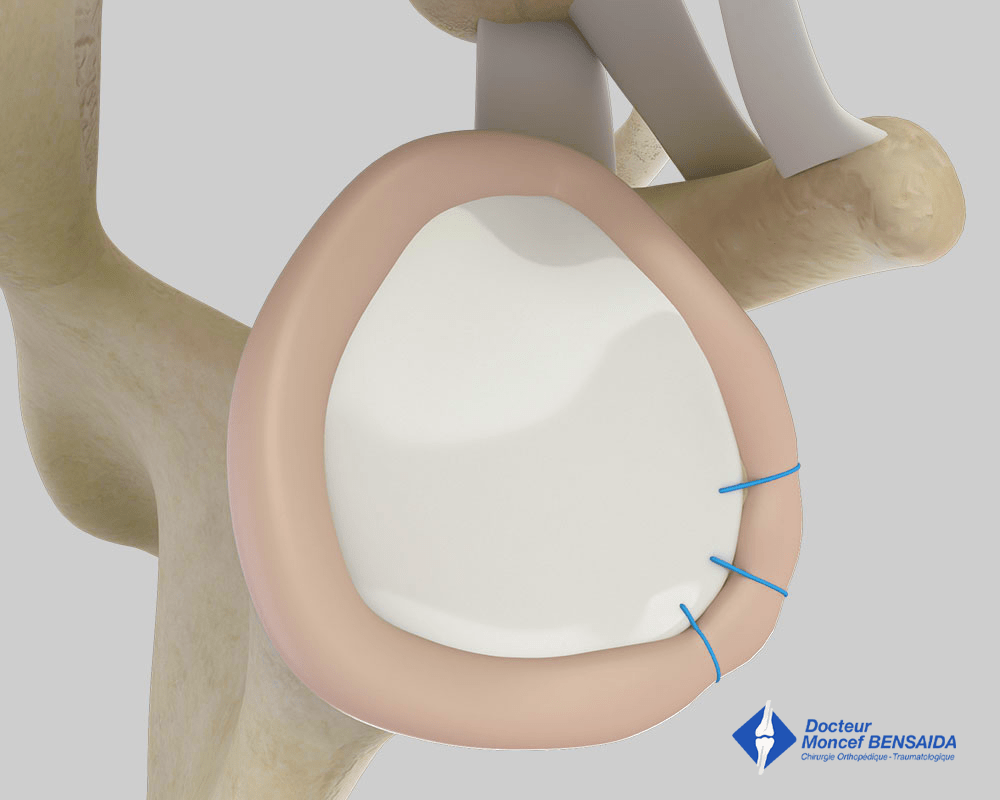
Final appearance of the reinsertion of the labrum (lateral view)
What are the limits of the operation?
Bankart repair aims to stabilise the shoulder as much as possible. However, a dislocation is still possible, especially in the case of a major blow or a particularly violent movement. Relapse depends on the condition of the joint at the time of the operation and the use of the shoulder in daily life.
The relapse rate after a Bankart procedure is approximately 10 to 15%. This can be decreased if the operation is only performed for recent instabilities with no bone damage in patients who do little sport and have no laxity.
What are the risks if left untreated?
If left untreated, there is a risk that the shoulder will dislocate more and more frequently with increasingly trivial movements. These dislocations cause increasingly severe damage that can result in the poor ageing of the shoulder (osteoarthritis) and make the surgery less effective.
THE OPERATION
Before the operation
Before the operation, a pre-anaesthesia consultation and a pre-operative assessment are conducted to check the patient is physically apt to undergo the operation and minimise the risk of postoperative complications.
The operation
The operation takes place in an operating theatre in compliance with strict standards of cleanliness and safety. The patient is placed on their side, and mild traction is applied to the arm on the side to be operated on. The operation lasts about 1 hour and is carried out under general anaesthesia, which is often combined with an interscalene nerve block. This additional anaesthetic maintains the shoulder and arm numb for several hours and limits postoperative pain.
The procedure is performed arthroscopically, a minimally invasive surgical technique that enables the operation to be carried out through 2 to 3 small incisions 5 millimetres in length around the shoulder. A miniaturised camera is inserted in the joint so the procedure can be followed on a screen.
After the operation
The shoulder is numbed with an interscalene block for 12 to 18 hours. Medication and ice also provide effective postoperative pain management.
The surgery can be performed as an outpatient procedure (leave hospital the day of the operation) or with a short stay of 1 to 2 days. The patient can return home when discharged.
The shoulder is kept in an orthopaedic sling for 6 weeks. Gentle, passive rehabilitation begins early in the week following the operation to stop the shoulder from getting stiff. It is then intensified from the 6th week after the operation and is often completed in the 3rd month after the operation.
When the patient is discharged from the clinic, a consultation with follow-up x-rays is scheduled with the surgeon 4 to 6 weeks after the operation to check there are no early complications, especially infections.
A second check-up is generally recommended approximately 3 months after the operation.
The duration of medical leaves depends on the patient’s profession but generally varies between 1½ and 2 months. It is longer for manual work.
Driving can be resumed 2 months after the operation.
Sports can be resumed using the shoulder operated on approximately 4 to 6 months after the operation.
RISKS LINKED TO THE OPERATION
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation. However, in the case of severe bleeding during or following the operation, another operation to stop the haemorrhage or a blood transfusion may be required.
Blood clots can form in the veins in the arm (thrombophlebitis) or lungs (pulmonary embolism). If the anaesthetist considers the risk high, you may be given a treatment to prevent this.
In rare cases, the shoulder remains stiff, hot, and painful for several months after the operation. This complication, known as algodystrophy or Chronic Regional Pain Syndrome (CRPS), is unpredictable and sometimes takes a long time to heal.
Other rarer complications can also occur. Blood vessels (arteries, veins) can be accidentally damaged and will require vascular surgery (bypass). Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.