ANTERIOR CRUCIATE LIGAMENT RECONSTRUCTION (KENNETH-JONES)
Anterior cruciate ligament (ACL) ligament reconstruction using the Kenneth-Jones technique is an orthopedic surgical procedure used to repair or reconstruct the anterior cruciate ligament of the knee, a ligament important for the stability of the knee joint. This procedure is usually performed when the ACL is severely damaged, torn, or ruptured due to a sports injury, accident, or other causes.
ACL ligamentoplasty process using the Kenneth-Jones technique:
- Anesthesia : The patient is usually placed under general anesthesia for the procedure.
- Site preparation : The surgeon cleans the operating area and disinfects the skin around the knee to reduce the risk of infection.
- Graft Harvesting : In this technique, the surgeon usually removes a piece of tendon from the patient himself, often the patellar tendon or quadriceps tendon, to serve as a graft. This tendon will be used to reconstruct the ACL.
- Tunnel preparation : The surgeon creates tunnels in the femur and tibia bone, through which the graft will be inserted.
- Fixation of the graft : The graft is inserted into the bone tunnels and secured in place using screws or other fixation devices.
- Suturing and Closure : Once the graft is correctly positioned, the surgeon sutures the skin and closes the incision.
- Rehabilitation : After the procedure, the patient begins a rehabilitation program supervised by a physiotherapist. This aims to restore strength, stability and mobility to the knee, as well as minimize the risk of complications.
ACL ligament reconstruction using the Kenneth-Jones technique is a complex surgical procedure that aims to restore knee stability, reduce pain and allow the patient to regain normal function of the knee joint.
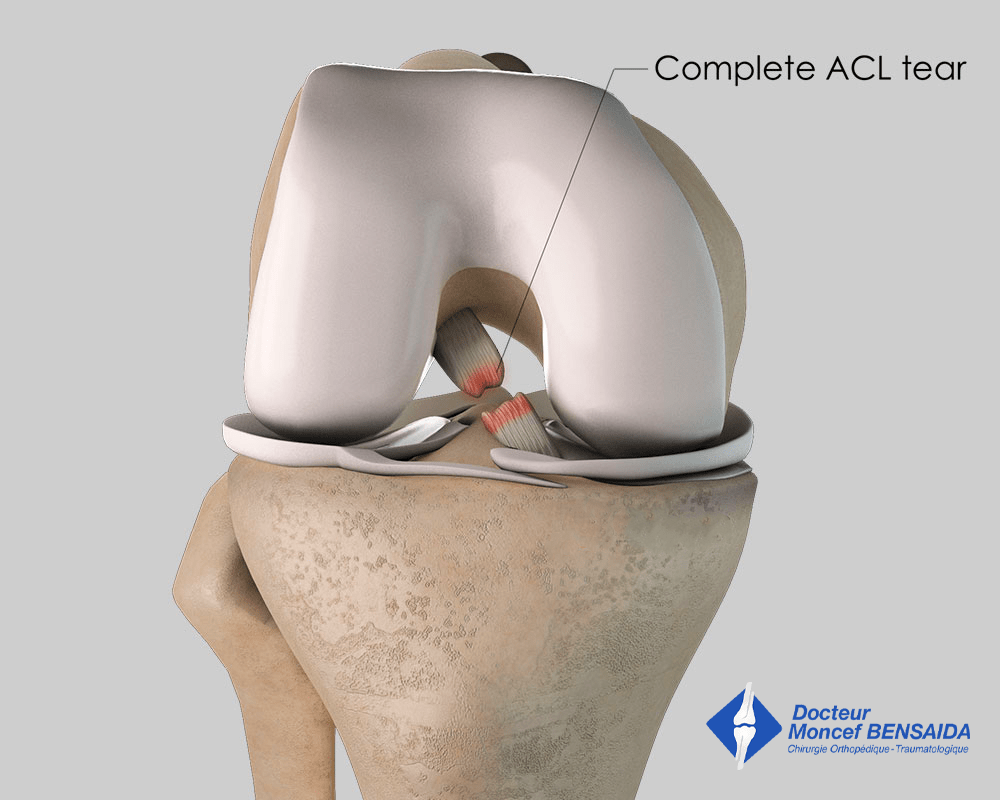
WHAT IS THE PROBLEM?
Under normal conditions, the knee is a stable joint and so dislocation is extremely rare. Anatomical components called ligaments ensure knee stability. Ligaments are like relatively inelastic ropes connecting the different bones in the knee.
The anterior cruciate ligament is located in the middle of the knee between the femur and the tibia. It stabilises the knee during pivoting, in other words, movements involving weight-bearing and rotation of the knee.
An anterior cruciate ligament tear or sprain most often occurs during a sports trauma as a result of twisting (football, rugby, ski…) or hyperextension (kicking into thin air) of the knee.
The consequences of an anterior cruciate ligament tear vary from one patient to another and it primarily develops in the following ways:
- The patient develops chronic anterior instability. The knee feels insecure during some movements and can give way. This instability can reveal itself during sports activities or daily life, during a sudden change in direction or on the stairs. It can develop soon after the trauma or later.
- The patient does not complain. The knee remains stable, especially thanks to the menisci, which are thus put under greater strain and can subsequently tear.
WHAT EXAMINATIONS ARE NECESSARY?
Immediately after the sprain, knee x-rays need to be performed to rule out a joint fracture of which the initial symptoms are very similar to an anterior cruciate ligament tear.
Once a fracture is ruled out, the patient must be examined by a doctor. A clinical examination immediately after a knee sprain is difficult due to the pain and often requires a reassessment two weeks later once the swelling has gone down and the pain receded. Most often, a clinical examination is sufficient to diagnose an anterior cruciate ligament tear. However, it is customary to perform a Magnetic Resonance Imaging (MRI) scan to confirm anterior cruciate ligament damage and highlight any other potential damage, especially to the menisci.
The surgeon may also request other knee x-rays to see if there is any cartilage wear, which can modify the indication or the type of operation proposed.
Finally, the surgeon may request dynamic x-rays (TELOS) or a GeNouRoB® examination to assess anterior knee laxity caused by the anterior cruciate ligament tear.
WHAT TREATMENTS ARE AVAILABLE?
Medical treatments, orthoses, and rehabilitation
In the days following the trauma, the knee is swollen due to the blood from the ligament tear making it difficult to bend the knee.
Walking is also difficult due to the sprain and quadriceps activation failure, which means the muscle cannot contract and no longer blocks the knee as it would normally.
The initial treatment must therefore act on all these symptoms.
The pain is treated with analgesics and anti-inflammatories. It is also recommended to put ice on the knee 4 to 6 times a day for the first few days following the trauma. When the knee is extremely taut and painful, the doctor can carry out an aspiration of the knee with a syringe to drain the bruise and thus relieve the pressure inside the joint.
A rigid brace (orthosis) will also be worn the aim of which is twofold: stop the knee giving way every time you put weight on it due to the quadriceps activation failure and help any torn lateral ligaments to heal at the same time as the anterior cruciate ligament.
Rehabilitation can begin early to recover joint range of motion and strengthen the quadriceps muscle.
When is surgery necessary?
→ Patients presenting an unstable knee
Anterior cruciate ligament rupture results in anterior knee instability. In some cases, the instability leads to a feeling of insecurity for the patient when putting weight on the knee; it feels as if it could give way. In other cases, this instability leads to the knee giving way, potentially resulting in a fall.
When the patient complains of instability, a ligamentoplasty (anterior cruciate ligament reconstruction) can be proposed.
Whether there is knee instability or not, a ligamentoplasty is proposed from the outset for some professions involving working at height (e.g. roofer), as the knee giving way could have dramatic consequences in the case of a fall.
→ Patients not presenting an unstable knee
In some cases, the knee remains stable, especially thanks to the menisci which have a dual role: ensuring knee stability and absorbing some of the strain to protect the knee from osteoarthritis. An anterior cruciate ligament tear puts the menisci under greater strain, increasing the risk of a meniscal tear. In young patients, this damage is linked to a risk of early knee osteoarthritis, which means anterior cruciate ligament reconstruction may be necessary in young patients to spare the menisci and indirectly prevent the onset of early knee osteoarthritis. In patients who do not complain about anything, this is called “preventive” surgery. In the latter case, it is necessary to weigh up the need for surgery, as this operation does not offer much hope for the patient in the short term but offers benefits in the medium and long term.
Consequently, in patients under 30 years with no knee instability, we tend to propose anterior cruciate ligament reconstruction. For patients between 30 and 40 years, we tend to operate when the knee is under a lot of strain (athletic patients doing pivoting sports: football, rugby, handball, judo, ski…).
The surgery proposed
An anterior cruciate ligament ligamentoplasty consists in reconstructing the ligament.
When is the best time to operate?
The best results are achieved when the ligamentoplasty is performed on a knee that has recovered from the initial sprain following rehabilitation sessions to reduce the swelling and recover normal mobility. The surgery is, therefore, elective and is generally carried out several weeks after the initial trauma. However, the best results in terms of controlling knee laxity are obtained if the operation is performed in the first 6 months after the trauma.
More rarely, the initial sprain is combined with a bucket handle meniscal tear causing the knee to lock during bending. In these circumstances, rehabilitation of the knee is not possible and the procedure must be performed rapidly to treat the meniscal tear at the same time as the anterior cruciate ligament ligamentoplasty and thus unlock the knee.
What are the risks if left untreated?
In the absence of surgery, there may be numerous consequences. The knee can become very unstable and it will be impossible to do some sports. Furthermore, the menisci may tear causing pain and even clicking of the knee. Ultimately, in the case of significant meniscal damage, osteoarthritis can develop.
THE OPERATION
If surgery is scheduled, the patient must consult an anaesthetist to determine the most appropriate anaesthesia with regard to the patient’s state of health. The anaesthesia will be either general (patient unconscious) or regional (spinal block) where only the lower part of the body is anaesthetised.
The operation takes place in an operating theatre in compliance with strict standards of cleanliness and safety. The patient is placed supine on an operating table and a tourniquet is placed around the thigh.
The main procedure: anterior cruciate ligament reconstruction
As the anterior cruciate ligament cannot be repaired, it must be reconstructed using a graft or plasty. With the Kenneth-Jones (KJ) technique, the graft is harvested from the patellar tendon located between the patella and the tibia (leg bone) through a vertical incision of 6 centimetres on the anterior side of the knee. The tendon can sometimes be harvested through two vertical incisions 2-3 centimetres each.
The patellar tendon is harvested with two strips of bone, one from the patella and the other from the tibia.
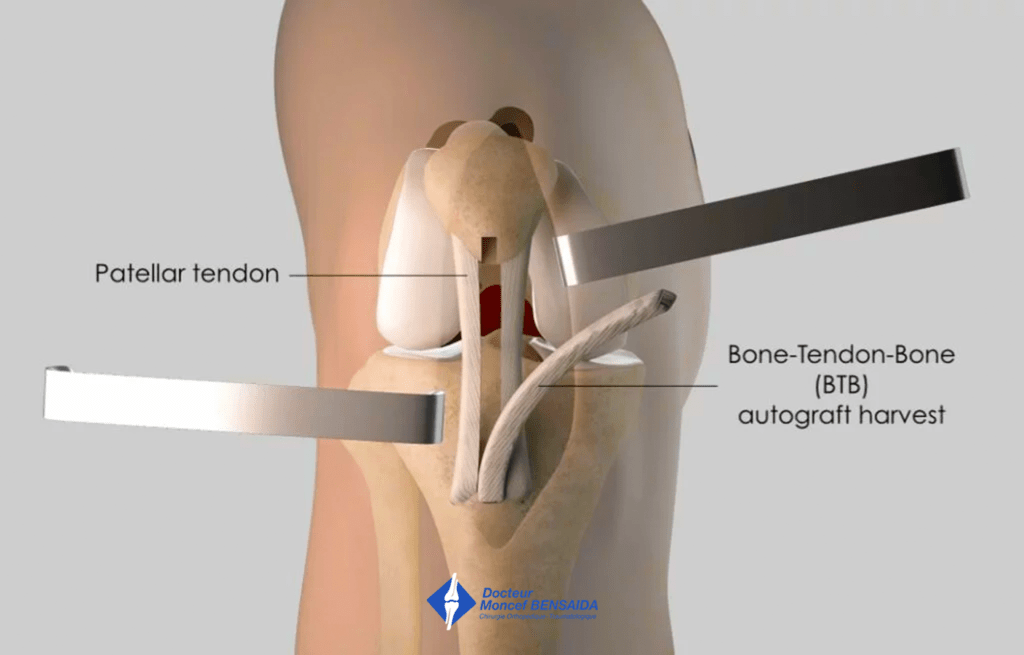
Harvesting of bone-tendon-bone graft
The next step is performed using arthroscopic surgery, a minimally invasive surgical technique that enables the operation to be carried out through two small incisions 5 millimetres in length located on the anterior side of the knee. A miniaturised camera is inserted in the joint so the procedure can be followed on a screen. The patellar tendon harvested at the start of the operation is inserted in the joint where it is fixed in bone tunnels created by the surgeon in the anterior cruciate ligament insertion sites on the femur and tibia.
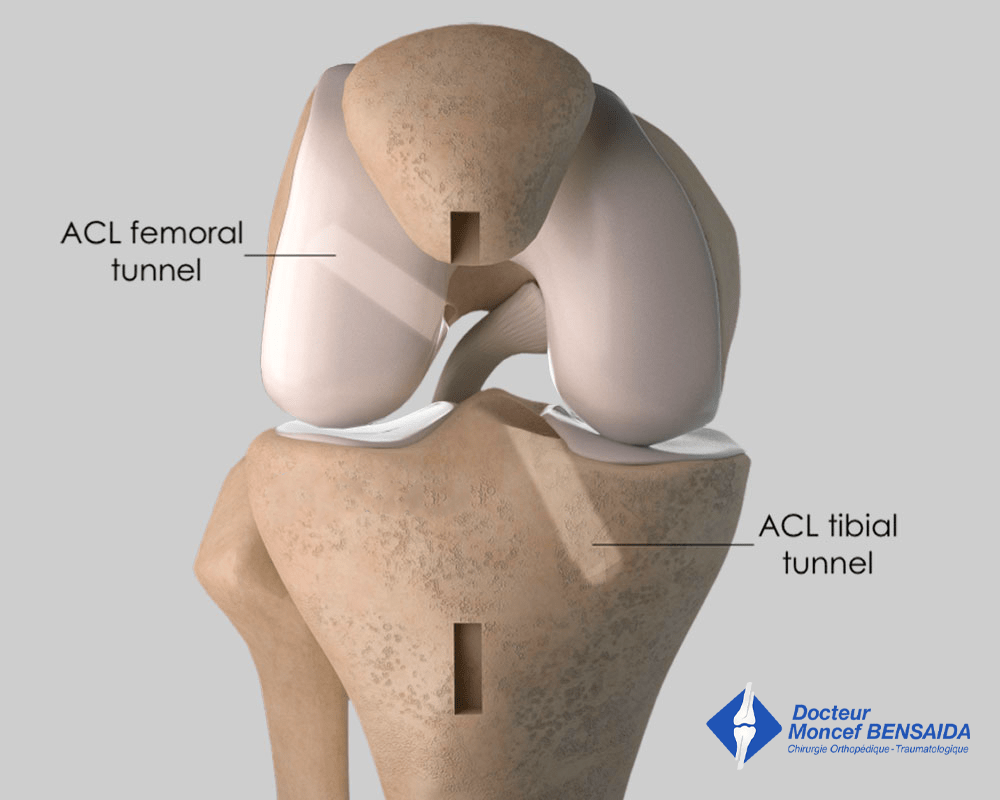
Creation of bone tunnels
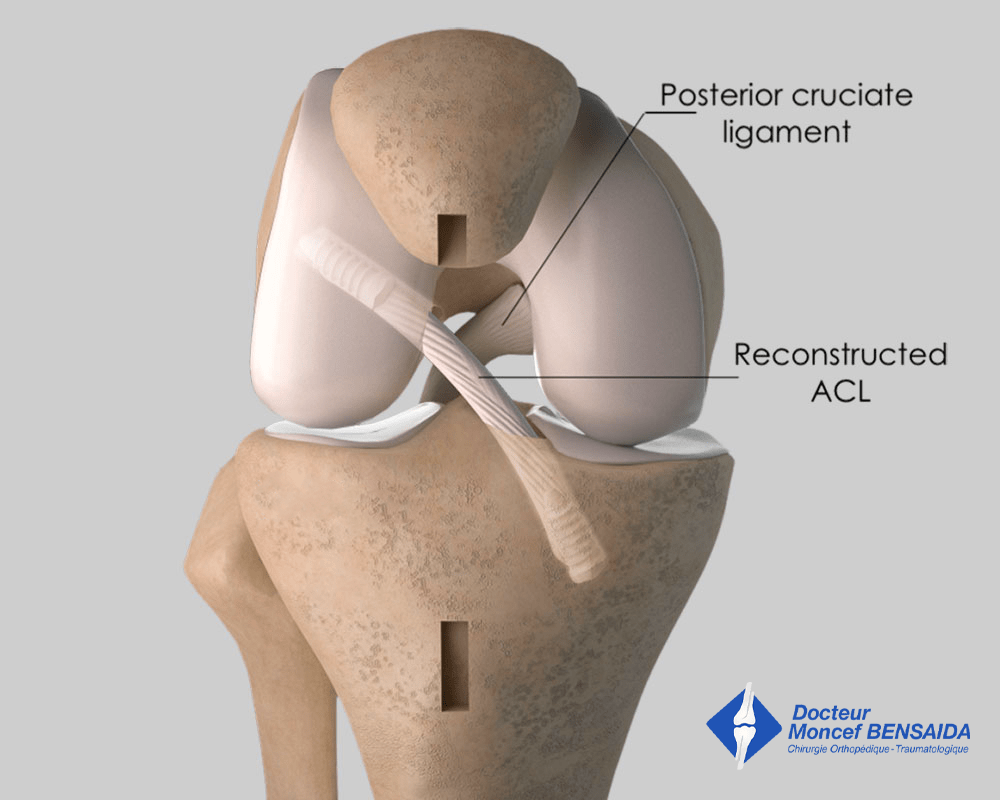
ACL reconstruction with patellar tendon: final appearance
Additional procedures
In some cases, in patients with extremely severe ligament laxity resulting in very flexible joints or good athletes involved in pivoting sports (football, rugby, ski, judo…), the surgeon can decide to combine ACL reconstruction with anterolateral ligament (ALL) reconstruction to help improve postoperative knee stability. This additional procedure requires an external incision of 5 centimetres to remove a band of tissue called Fascia Lata, of which the harvest is inconsequential.
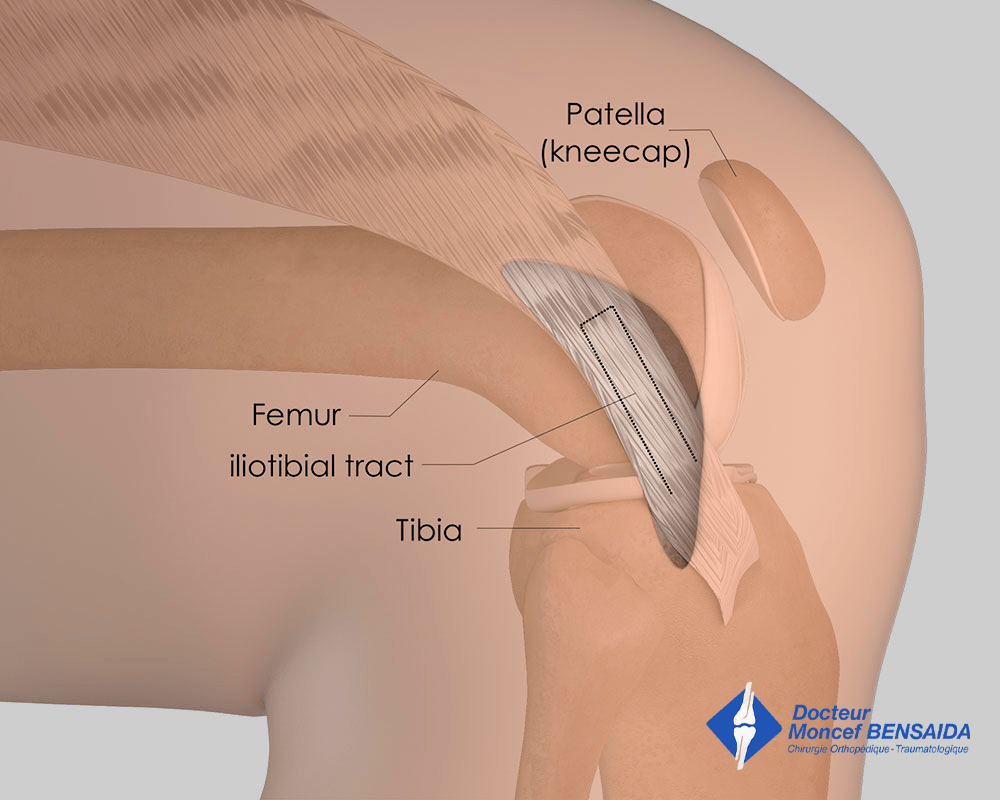
Reconstruction of the anterolateral ligament: harvesting of the iliotibial band
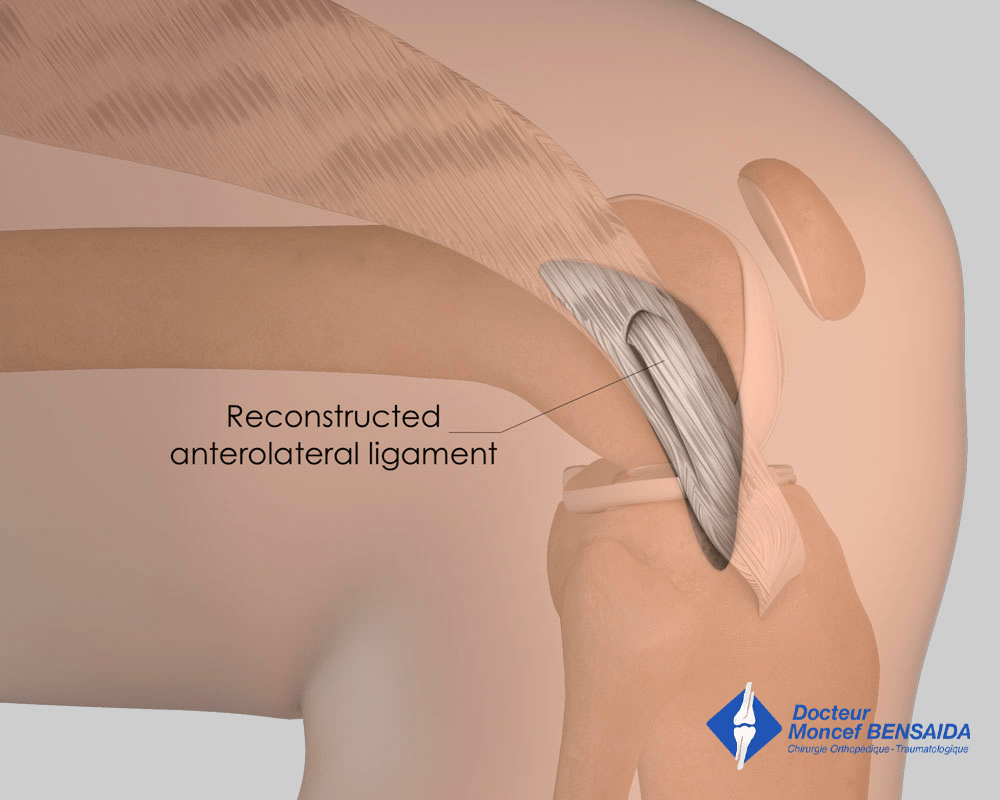
Reconstruction of the anterolateral ligament: final appearance
In addition, any meniscal damage can be treated during the operation. The meniscus is repaired or the damaged part removed.
Before closing up, a drain (Redon) is often inserted in the incision to drain the blood and prevent the formation of a haematoma. This drain is generally removed just before the patient is discharged.
In general, the procedure lasts between 40 minutes and 1 hour 15 minutes.
No blood transfusion is necessary for this operation.
AFTER THE OPERATION
The initial pain is usually managed well with drugs or even a nerve block (placed in the operating theatre by the anaesthetist), which keeps the knee numb for several hours after the operation.
This operation is usually carried out as an outpatient procedure or during a short stay of fewer than 2 days.
Weight-bearing is allowed from the outset but must be aided with crutches for 3 weeks. A knee brace is often used when going out for the first month after the operation. However, a brace is not necessary at home.
During the first month after the operation, you must reduce your level of activity. A nurse will visit you at home to change the dressings and administer the anticoagulant injections for the first three weeks.
Rehabilitation begins in the days following the operation. The initial aim is to wake up the muscles, help the swelling of the knee go down, and recover flexibility.
A check-up is scheduled one month after the procedure to assess recovery and progress made, as well as to adjust rehabilitation if progress is not as expected. Other check-ups are usually scheduled during the 3rd and 6th month after the operation.
You must remember that it is normal for your knee to remain swollen in the weeks following the operation. The pain will gradually fade over time and you will usually recover good knee function for daily life 6 weeks after the operation. However, this is an average and may take longer for some patients.
RESUMING WORK AND SPORT
The duration of medical leave depends on the patient’s profession and the type of operation but is usually between 1 and 3 months.
Sport can be resumed progressively. An exercise bike can be used soon after the operation. Running on flat ground (athletics track or treadmill) can be resumed from the 4th month and on any ground from the 6th month. Swimming with a flutter kick can also be resumed from the 3rd month. Most sports can be resumed after 6 months; however, particular caution must be taken with pivoting sports (football, ski, judo) for which it is necessary to wait until the 9th month.
The return to sport may differ depending on the additional procedures performed on the meniscus or cartilage.
RISKS LINKED TO THE OPERATION
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics. Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation.
Knee surgery also increases the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections) are prescribed for 3 weeks following the operation.
In rare cases, the knee remains stiff, hot, and painful for several months after the operation. This complication, called algodystrophy or complex regional pain syndrome (CRPS), is unpredictable and sometimes takes a long time to heal.
Quite often, a small area of skin around the incision made to harvest the tendon or a larger area of the leg remains numb after the operation as a result of the internal saphenous nerve being stretched. Feeling is usually recovered within 6 months. More rarely, the loss of feeling persists but is not bothersome.
Finally, hypertrophic scar tissue (fibrosis) can appear at the site of the plasty preventing total extension of the knee. This is called the Cyclops syndrome and is often linked to problems with initial rehabilitation and may require another arthroscopy to remove the scar tissue and thus restore total knee extension. This complication is rare but must be verified with an MRI if it is suspected.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.